First of all congratulations on your new born baby, or congratulations on your pregnancy and upcoming baby! If you have not yet had your baby spoiler alert ahead! If you've had your baby, you've made it through labor and birth (I specifically do not use the word delivery because a baby does not get "delivered" no matter if you had a cesarean section or vaginal delivery.) Not sleeping through the night has become a reality; if you chose to breastfeed you may be navigating the challenges of latching and positioning during breast feeding and also figuring out if you can eat while breastfeeding (I know I was!); you're checking to make sure your baby is still breathing when they are sleeping; you're freaking out about cutting their nails but they keep scratching their face so you know you have to do it; you're trying to figure out if you can ever go to the bathroom by yourself and how you will ever shower again; the list goes on. What a new world you have entered! And just like that, although the days are long, the weeks are fast and 6 weeks have gone by and you now have your "6 week check-up." You're both excited and terrified for someone to look at your vagina but you are hoping to feel some relief afterwards by them telling you everything is normal. So, while you are reluctant, you pack up the diaper bag, put the baby in the car seat, and head out for your appointment. And you pause and remember when it didn't take you 40 minutes to get out the door!
So, let me break it down for you. Most commonly, your OBGYN will have you lie down, they will feel inside of your vagina and check the tissues and tell you you can have intercourse. That's it! Yep, really that is it. Now, some midwives and OBs do do a little more checking and they may even have you do a kegel (pelvic floor muscle contraction) and say your strength is good. They may even ask you if you are leaking any urine. Some of them may tell you that leaking urine is normal at this point. They may ask you if you are still bleeding and how much.
Here's what they won't tell you: whether or not sex will be painful; how strong your pelvic floor muscles are and if you need to start doing some exercises to strengthen them and what these exercises would look like; if your pelvic floor muscles are hyperactive; do you have prolapse? if your abdominal muscle tissues have widened and what to do about that; what level of activity is normal to return to at 6 weeks and how to get back to what you used to do; what types of exercises you can do and what level of increased bleeding while doing them is normal; if you are leaking urine when are you leaking urine and what types of treatments you can try to address this; if you had a cesarean section what to do about your scar and how much abdominal pain is normal; if your back hurts and what to do about it; the list goes on!
All of the above "what they won't tell you" is what we will tell you if you come to see a pelvic health physical therapist. It's that simple. We will give you a comprehensive understanding of what's normal, when it's not normal, when it becomes abnormal, and specific exercises and everyday life activities you can do to to keep your healing on track and get back to being as active as you want while preventing a lot of long term post-partum complications.
Now, I'm going to break it down for you again, line item by line item:
Will sex be painful?
Most likely yes. Nearly 90% of women report pain the first time they have sex. While this is very common, it is not normal for this pain to persist. Most of the time, the pain with intercourse will get better over time, but if you continue to have pain with intercourse each subsequent time that you try, this is not normal and may indicate that you have an impairment in your pelvic floor muscles that needs to be treated. There are 2 requirements for intercourse to not be painful: (1) vaginal lubrication from arousal, and (2) the vaginal canal needs to lengthen and open and become engorged with blood. If you have a lot of scar tissue from tearing during birthing your child, this may restrict the vaginal canal from lengthening. Also, if you have pelvic diaphragm muscle hyperactivity, this could be restricting the vaginal canal. It is normal to have decreased lubrication in your vagina when you are breastfeeding because you have decreased estrogen when you breastfeed which causes vaginal dryness. Try a lubrication if you are feeling like you have dryness in your vagina.
Are your pelvic diaphragm/floor muscles strong?
Not always, but they are most likely weak at your 6 week check-up. If you had tearing (approximately 1/3 of vaginal births results in some injury to the levator ani muscle [the deepest layer of the pelvic diaphragm muscles]), then they may be even weaker. You carried a baby in your pelvis for 40 weeks and that puts a lot of pressure on your pelvis, the organs in your pelvis, and the pelvic diaphragm muscles. You can begin kegels immediately after you deliver your baby. Yes, that's right, you can start doing contractions right after your baby is born as long as it's not too painful. How you do these contractions is important. You always want to do pelvic diaphragm muscles when you exhale because this is how your body is naturally designed to function best. Its the elastic recoil of the diaphragm that occurs when you exhale that triggers a contraction of first the pelvic diaphragm muscles and then the lower abdominal muscles (we know this from real time ultrasound imaging). You should also do them with a lower abdominal muscle contraction because the transversus abdominis muscle is best friends with the pelvic diaphragm. And you may even want to contract your glutes when you do a pelvic diaphragm contraction because they are very close friends. You can do the exercises lying down if you think you need to concentrate. You can do them in sitting, possibly on a ball so you get some feedback from the ball when you contract. You can do them in standing. You can do contractions with a hold that lasts as long as your exhale. You can do some longer holds at about 50% level of effort to train endurance. And you can do some quick and strong contractions to train the pelvic diaphragm muscles for power which is ultimately what they need to prevent leaking with coughing, sneezing, and laughing. A physical therapist will be able to come up with a comprehensive exercise program to keep your pelvic diaphragm muscles strong and prevent post partum complications such as leaking urine and pelvic pain.
Are your pelvic floor muscles hyperactive?
The only way to objectively tell if your pelvic floor muscles are hyperactive is to use a biofeedback machine. The biofeedback machine has a grounding electrode and 2 other electrodes that are placed on both sides of the anus. The biofeeback machine reads the activity of the muscle and tells us what the resting tone of the muscle is when you relax. We know that normal resting tone of the pelvic diaphragm muscles is supposed to be between 2-3 microvolts. If you relax your pelvic diaphragm muscles and the resting tone is above 2-3 microvolts, then you have hyperactivity. This means that your pelvic diaphragm muscles do not have the ability to fully relax, they are "resting" in a shortened and tightened position. They need to be trained to relax with specific breathing (diaphragmatic breathing, specifically on the inhale) and lengthening exercises such as perineal bulging.
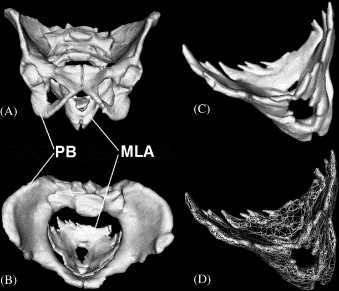
Do you have prolapse?
Prolapse happens when your internal pelvic organs collapse downwards. There are different degrees of downward collapse. This collapse downwards can happen because you are not managing pressure well (holding your breath or straining to go to the bathroom), from the pressure of carrying a baby in your pelvis for 40 weeks, from increased laxity of your internal pelvic ligaments, and from weak pelvic diaphragm muscles. There are 2 components to prolapse of which I like to use the boat in water analogy. The boat is your internal pelvic organs. The water if your pelvic diaphragm muscles. The ties to the dock are your internal ligaments that attach the internal organs to different body structures in your pelvis. If the pelvic diaphragm muscles are weak, there is not enough water under the boat to support it and keep it buoyant and this will then put a lot of strain on the dock ties or the internal pelvic ligaments. If there is a lot of laxity in the internal pelvic ligaments or the dock ties are loose, then you need a lot of water under the boat to keep it afloat. Depending on what the root cause of the prolapse is, a physical therapist can give you exercises to address prolapse and prevent it from worsening.
Have your abdominal tissues widened?
The answer is 100% yes! At some point during your 3rd trimester your abdominal muscles widened to accommodate your growing baby! This is 100% normal! For some women, these muscles just go right back to where they were before they had a baby. A study that was done showed that this happened as soon as 72 hours after birthing their baby without doing any specific exercises targeted at diastasis! For some women, the abdominal muscles stay widened and this is considered normal at the time of your 6 week check-up. Abdominal tissue widening becomes abnormal when you are 12 weeks post-partum. Most of the time, the reason why they are staying widened is because of one of the following: are you continually stressing the muscles (are you doing a lot of overhead lifting and flaring your ribs out?); are you constipated and straining to have a bowel movement?; are you holding your breath when you do anything that requires effort? are you overactive in your rectus abdominis and oblique muscles but really weak or poor at activating your transversus abdominis muscle?; are you jack-knifing when you get out of bed?; are you doing exercises that are making your abdominal muscles tent or bow out? You can begin doing exercises for your diastasis rectus immediately after you delivery your baby. See my blog post about diastasis rectus abdomins [link] for more information.
What types of exercises can you do? What if I am bleeding? What if I am leaking?
I know! I'm doing a three for one! I am combining several key points here because they go hand in hand. This is a more challenging question to answer directly, but I will do my best. The idea that you will be able to resume all pre-pregnancy activities at 6 weeks is generally a completely false statement. Nobody seems to know how this timeframe was decided upon in the medical community and there is more and more consensus that this expectation is not realistic and not safe. Your body needs to heal and recover from carrying a baby in your pelvis for 40 weeks and all of the hormonal changes that came along with it. There is no line in the sand. Some women, they may try some longer walks at 6 weeks post partum and for others a walk around the block feels like enough. Ultimately you need to listen to your body and trust what you feel to know and gauge the activity level that is right for you. Generally speaking, if you were very active before and during your pregnancy, you may be able to return to activity sooner than someone who was not as active. If you had more tearing during the delivery of your baby, you may need more time to rest. If you are doing activities and having any heavy bleeding or clotting, this is a sign that the activity you are doing is too much and you need to pull back. If you are leaking urine when you do an activity, having a lot of feelings of pelvic heaviness, or having a lot of abdominal or back pain and you can't modify your form or strategy to eliminate those symptoms then you need to pull back. A physical therapist would be the best person to advise you on what exercises to try and what to look out for.
What if I had a cesarean section?
Many women think that because they had a cesarean section (c-section), they are immune to pelvic floor/diaphragm issues. False! If you had a c-section, you carried a baby in your pelvis for 40 weeks which is a really long time! You had increased weight in your pelvis and your pelvic ligaments and muscles stretched just like every other moms! So, while you didn’t have the type of direct trauma you would if you had a vaginal birth, it is still very much worth seeing a pelvic health physical therapist and get an evaluation to make sure you stay in the clear! Additionally, your abdominal muscles were cut through, and now your body needs to lay down scar tissue to heal the incision. Scar tissue is generally a lot stickier and less flexible than other tissues in your body. It requires stress in specific directions in order to align with the fibers of tissues that it is repairing to allow the tissues to move freely and normally. It is recommended by physical therapists that all women who have had a c-section receive some sort of tissue mobilization of their c-section scar.